Musculoskeletal ultrasound (MSK) is a new ultrasound examination technology that has emerged under the background of the continuous advancement of imaging technology in recent years. Ultrasound used to diagnose diseases of the musculoskeletal system can clearly display superficial soft tissue structures such as muscles, tendons, ligaments, and peripheral nerves, and the lesions that occur, such as structural abnormalities caused by inflammation, tumors, injuries, and deformities.
Musculoskeletal ultrasound is highly pertinent and supports multi-angle real-time dynamic image scanning, which can be dynamically completed under different movement and body positions of the patient, and supports bilateral comparison at the same time, which is conducive to identifying lesions. The ability of ultrasound to display soft tissue lesions is comparable to that of MRI, and it can finely distinguish muscle and superficial nerve anatomy. At present, physicians prefer to use portable ultrasounds for scanning, which are small and portable, have strong repeatability, and are convenient for monitoring treatment effects. It can effectively improve patient acceptance and reduce hospital procurement costs.
Below we will analyze and discuss a typical case of musculoskeletal ultrasound: carpal tunnel syndrome.
The structure of the carpal tunnel:
The carpal tunnel is a bony fibrous sheath formed by the transverse carpal ligament and the carpal bone. It is about 2-2.5 cm long and 2.5 cm wide. Carpal and intercarpal ligaments.
The contents of the carpal tunnel include 9 tendons and 1 median nerve, the latter lying below the transverse carpal ligament, superficial to the 2nd and 3rd flexor tendons, and medial to the flexor hallucis longus tendon. In the anatomy of the palm, the median nerve innervates the radial half of the 1st, 2nd, 3rd, and 4th fingers, and the radial motor innervates the thenar muscle.

What is carpal tunnel syndrome (CTS)?
Carpal tunnel syndrome, also known as median nerve entrapment syndrome, refers to a group of symptoms and signs caused by compression of the median nerve as it passes through the carpal tunnel. Patients often have pain and paresthesia in the innervated area of the median nerve, and occasionally weakness. CTS is the most common compressive focal mononeuropathy clinically.
What are the warning signs of carpal tunnel syndrome?
Carpal tunnel syndrome often occurs between the ages of 30 and 50. It mainly manifests as compression of the positive peripheral nerve, numbness, tingling or burning sensation in the thumb, index finger and middle finger. According to clinical symptoms, carpal tunnel syndrome can be divided into three stages. In the early stage, patients often wake up painfully at night, and in severe cases, it may be accompanied by radiating pain from the wrist to the shoulder. In the mid-term, patients will also have motor dysfunction such as instability in holding objects on the basis of tingling and numbness. In advanced stages, the thenar muscles may atrophy, and trigger points may appear in multiple places on the shoulder, such as subscapularis and anterior scalene muscles.
What is the main cause of carpal tunnel syndrome?
The causes of median nerve entrapment are various. Swelling of the tendon, tenosynovitis or even cysts may cause entrapment of the median nerve. In addition, the hyperplasia of the wrist joint and carpal bone, and the osteoarthritis of rheumatoid and gout patients will also cause the space in the cavity to become smaller, and the median nerve will be compressed. Therefore, it is very important to find the cause of median nerve entrapment when diagnosing carpal tunnel syndrome.
The etiology of carpal tunnel syndrome can be divided into two categories: systemic factors and local factors.
1. Local factors
Decreased carpal tunnel volume: thickened transverse carpal ligament, carpal bone variation
Increased carpal tunnel content: synovial hyperplasia around the tendon, carpal fracture and dislocation, etc.
Reasons for position: hyperextension or hyperflexion of the wrist joint, etc.
2. Systemic factors
Neurogenic: Diabetic neuropathy
Inflammatory response: rheumatoid arthritis
Fluid imbalance: pregnancy, hypothyroidism, menopause, etc.
What is the role of ultrasound in carpal tunnel syndrome?
The sonographic diagnosis of carpal tunnel syndrome
Ultrasound image of normal carpal tunnel: the median nerve in the carpal tunnel is elliptical in transverse section, with lower echo than the tendon, located deep to the transverse carpal ligament, superficial to the 2nd or 3rd flexor tendon and flexor hallux On the medial side of the tendon, the longitudinal section shows that the median nerve gradually becomes thinner as it travels to the distal end without compression.
Ultrasound image of carpal tunnel syndrome: Ultrasound shows that the median nerve in the distal carpal tunnel is compressed and flattened, the median nerve in the proximal carpal tunnel is thickened, and the local transverse carpal ligament bulges toward the palm side. A cross-sectional area >10 mm² can be diagnosed as carpal tunnel syndrome.
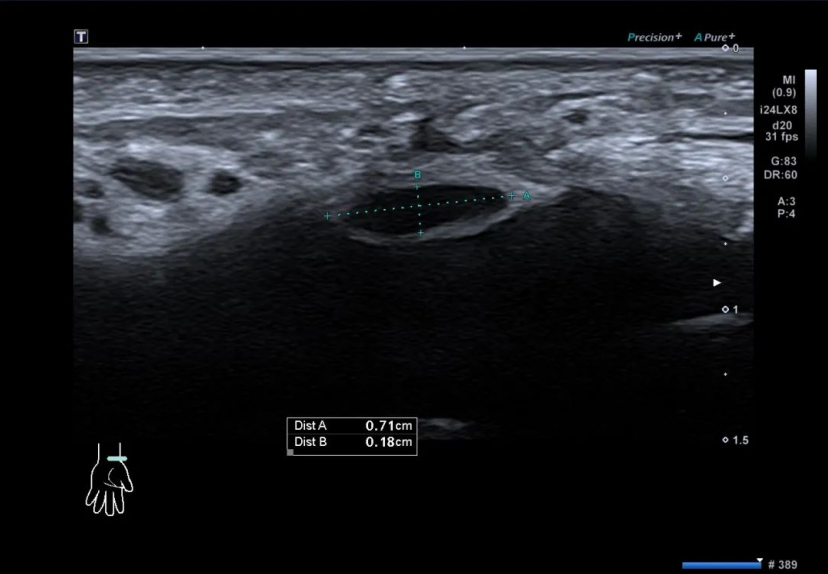
It is worth noting that, in order to identify the median nerve at the carpal tunnel and discover neuroanatomical variations more easily during ultrasonography, the median nerve can be first confirmed from the distal forearm between the flexor digitorum deep and superficial flexor digitorum, and then slowly move the short-axis view of the ultrasound towards the carpal tunnel to complete the examination.
Diagnosis can be made under ultrasound guidance in several ways
1. Median nerve flattening ratio
The ratio of the long diameter to the short diameter of the position where the median nerve is compressed is the flattening rate. KeberleM et al. set the diagnostic standard as 3.4[1] , and Buchberger et al. set the diagnostic standard as 4.2. [2]
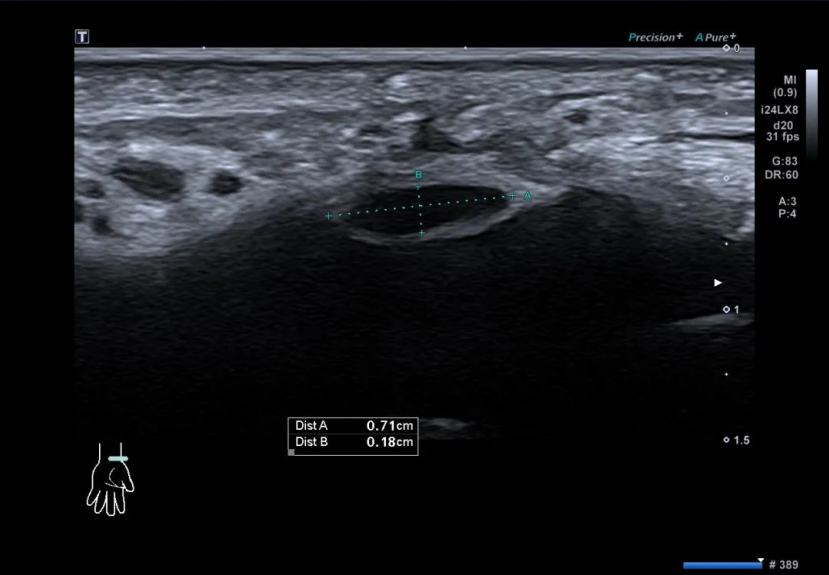
2. Median nerve cross-sectional area
The cross-sectional area of the median nerve is the most widely studied and recognized diagnostic index so far. El Miedany et al. studied the diagnostic value of measuring the median nerve CSA in different sections. When the cut-off value was 10mm², the sensitivity and specificity for diagnosing CTS were the highest, which were 97.9% and 100.0%, respectively.
3. Median Nerve Color Doppler
The blood supply of the median nerve is composed of epineurium, fiber bundles and the communication between them.
Under normal circumstances, Doppler ultrasound of the human median nerve will not detect blood flow signals (except for the persistent median artery). When the median nerve is damaged, the blood flow state of the median nerve will change to a certain extent. Judging the change of blood flow state by portable ultrasound can detect whether the median nerve is damaged in time.

4. Other observation indicators
The inner diameter of the MN, the thickness of the epineurium, the thickness of the transverse carpal ligament, the longitudinal compression sign (a sign of MN compression in the carpal tunnel seen in the longitudinal scan of the ultrasound probe), and the CSA difference (the difference between the CSA of the carpal tunnel plane and the proximal median nerve of the forearm) ) and so on can be used as auxiliary diagnostic indicators for carpal tunnel syndrome.
In the past clinical diagnosis, electrophysiological examination was considered the gold standard for diagnosis, but it could not show the structures around the median nerve, and could not further determine the etiology, resulting in relatively large application limitations.
Portable ultrasound has been widely used in clinical disease diagnosis. It can accurately observe the changes of the median nerve and surrounding structures in patients with carpal tunnel syndrome, provide evidence for etiology and quantitative diagnosis, improve the accuracy of diagnosis, and provide a reference for the selection of clinical treatment options.
Ultrasound-guided acupuncture-knife release of the transverse carpal ligament
1. Preparation: Under the guidance of ultrasound, observe the shape and positional relationship between the median nerve and the transverse carpal ligament, determine the needle insertion point, perform local anesthesia, and inject a small amount of liquid between the transverse carpal ligament and the median nerve to separate them.
2. Loosening: Insert the needle at the same needle insertion point, cut and release the transverse carpal ligament directly above the median nerve under the guidance of ultrasound, the incision line is parallel to the median nerve, and cut the transverse carpal ligament longitudinally from near to far 4-6 Next, peel off with a parallel swing. Physicians need to pay close attention to real-time ultrasound images to prevent damage to the median nerve. And then needle-push dressings protect the needle holes.
3. Precautions: Most doctors are used to releasing the short axis of the probe above the transverse carpal ligament for release. The disadvantage of this operation is that the range of release is relatively small, and it is prone to incomplete release. Therefore, it is recommended to place the probe on the long axis, and after finding the entrapment site, separate the analgesic solution and water between the normal peripheral nerve and the transverse carpal ligament, and then perform needle-knife release.
Wireless Portable Ultrasound Used in MSK
Musculoskeletal ultrasound has the advantages of real-time dynamics, convenient examination, and no radiation. Therefore, it gradually occupies an important position in the diagnosis and evaluation of musculoskeletal nervous system diseases. Musculoskeletal ultrasound technology can clearly display the structure of cortical bone, muscle, tendon, ligament and peripheral nerve, and determine the technique and scope of the lesion. Accurate treatment of lesions guided by ultrasound can provide more effective visual diagnosis basis for clinical practice.

The parts to be examined by musculoskeletal ultrasound are relatively superficial tissues, so there are high requirements for ultrasound probes, such as high resolution, clear layers, and the ability to display small blood flows. Viatom dual-head ultrasound can display the morphological changes and interaction forces of joints, bones, muscles and infrastructure in real time during active, passive or resistance movement of patients, which is helpful for the diagnosis of motion diseases and impingement syndrome.
Welcome to contact us for more cooperation details.
Reference:
- Technical advances in ultrasound and MR imaging of carpal tunnel syndrome:https://pubmed.ncbi.nlm.nih.gov/11003395/
- Keith MW, Masear V, Chung KC, Maupin K, Andary M, Amadio PC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478–2479.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4960212/