The heart is among the most critical organs in your body. It continuously pumps blood through the circulatory system, ensuring cells obtain a sufficient supply of blood and oxygen. Several conditions can impact the heart and its functions, leading to complications if you do not get a diagnosis and start with a treatment plan. This post will discuss Atrial Fibrillation, also known as A-fib. The condition, which impacts the heart, raises the likelihood of specific complications like heart failure and stroke.
Basics Of A-fib
Atrial fibrillation (A-fib) is a significant disturbance in the electrical activity of the heart’s atria and is a common form of rapid cardiac arrhythmia. It is characterized by the substitution of regular and organized atrial electrical activity with rapid and disorganized atrial fibrillation waves. To better understand A-fib, it is essential to examine its pathophysiology, consequences, and signs. Notably, the pathophysiology, consequences, and signs of A-fib can be classified into three distinct aspects, emphasizing the significance of the number three.
1. Three pathophysiological features
A-fib is characterized by three main pathophysiological features.
- Firstly, the irregular and disorganized electrical signals in the atria impair their ability to contract and relax effectively, leading to compromised pumping function and impaired cardiac performance. This abnormal atrial activity disrupts the synchronized contraction necessary for optimal blood flow and can result in reduced cardiac output.
- Secondly, the irregular conduction of rapid atrial impulses to the ventricles via the atrioventricular (AV) node causes highly erratic ventricular responses. This irregularity in ventricular rhythm and rate can lead to palpitations, a sensation of fluttering in the chest, and hemodynamic instability. The disruption of normal electrical conduction pathways can result in ineffective ventricular contractions, further compromising the heart’s ability to pump blood efficiently.
- Lastly, the presence of disorganized atrial activity fosters a favorable environment for the development of blood clots within the atria., particularly in the left atrial appendage. These intracardiac thrombi pose a significant risk as they can dislodge and travel through the bloodstream, potentially causing blockages in critical vessels and leading to serious complications such as strokes or organ damage.
2. Three main consequences
A-fib is associated with three primary consequences.
- Firstly, the irregular ventricular response manifests as symptoms like palpitations, fatigue, and general discomfort, significantly affecting the patient’s quality of life.
- Secondly, A-fib led to impaired atrial contraction, resulting in decreased cardiac output and reduced pumping capacity of the heart. This decline in cardiac function is particularly prominent in the presence of underlying structural heart diseases.
- Lastly, the disrupted blood flow dynamics within the atria increase the propensity for thrombus formation. Compared to individuals without A-fib, those with A-fib face a 15-fold higher risk of complications arising from thrombus formation, with strokes being the most prevalent, often leading to substantial disability.
3. Three crucial signs
During the physical examination of patients with A-fib, there are three crucial signs to consider.
- Firstly, the absolute irregularity of heart rhythm is a key indicator, as A-fib disrupts the normal cardiac rhythm, leading to chaotic atrial fibrillation. This irregularity can be detected through careful auscultation of the heart.
- Secondly, the variable intensity of heart sounds an important observation. The irregular and rapid atrial contractions in A-fib can affect the intensity of heart sounds, causing fluctuations during an examination.
- Lastly, the irregularity of arterial pulses is another significant sign. Due to the irregular heart rhythm, arterial pulses may exhibit an inconsistent rhythm or skipped beats. These signs play a vital role in diagnosing A-fib and provide valuable information for guiding appropriate management strategies for patients.
In summary, A-fib is a serious cardiac arrhythmia that has a wide-ranging and significant impact on cardiovascular health. Early detection and timely intervention play a vital role in the management of patients with A-fib.
Types Of Atrial Fibrillation
When diagnosing A-fib, it’s important to note that there are different conditions. Understanding the specific type of atrial fibrillation you have simplifies the process of comprehending what to anticipate and how treatment is expected to be effective.
Here is an overview of the different atrial fibrillation types that can develop:
- Paroxysmal A-fib: A common type of A-fib. This type involves episodes that come and go. The rapid heartbeat and other symptoms have a spontaneous onset but then disappear again within the next 24 hours. It is possible that you won’t manifest any symptoms during this stage, as paroxysmal A-fib is often asymptomatic.
- Persistent A-fib: When you have persistent A-fib, the condition also develops spontaneously but persists for longer than a week. Sometimes, persistent A-fib does not go away without medical intervention.
- Long-standing Persistent A-fib: If there is structural damage to the heart, then long-standing persistent A-fib can sometimes develop. This refers to atrial fibrillation that lasts for longer than a year.
- Permanent A-fib: If the treatments used for long-standing persistent A-fib do not help, the condition can sometimes become permanent. Current therapies used may be stopped at this point.
Mechanisms Of A-fib
There are various studies that explore the mechanisms of A-fib. For a long time, the multiple wavelet hypothesis has been used to describe the mechanisms of the condition. There are also those that propose a focal activation mechanism to be associated with A-fib. In this case, the mechanism describes the origination of A-fib from focal activity focused on a particular area. In focal activation, A-fib originates from the pulmonary vasculature.
Risk Factors Of A-fib
Age stands as the most significant risk factor linked to the condition. Increasingly, the older you are, the higher your risk of developing atrial fibrillation.
Other risk factors that you should also acknowledge include the following:
- Existing cardiovascular conditions, such as problems with the heart valves, increase the risk of atrial fibrillation.
- High blood pressure can also increase the risk of developing A-fib.
- Alcohol consumption has been linked to the activation of atrial fibrillation episodes.
- Individuals who have a family history of A-fib also demonstrate a higher likelihood of developing the condition themselves.
- Problems with the thyroid can affect the heart, increasing the risk of A-fib.
- People with other chronic conditions, such as lung disease, sleep apnea, and metabolic syndrome, are also at a greater risk.
Prevention Of A-fib
Consistently visiting your healthcare provider serves as an excellent preventive measure against A-fib. Your healthcare provider can do regular checkups by listening to your heart and ordering tests when they detect abnormalities in your heart’s rhythm.
Certain preventive measures can also be undertaken independently to mitigate the risk of A-fib. These include:
- If you smoke, consider quitting.
- Exercise regularly.
- Try to maintain a weight appropriate for your height and age.
- Consume meals that are high in nutritional value.
- Implement stress management techniques in your daily life.
Diagnosis Of A-fib: ECG
A-fib is a common cardiac arrhythmia characterized by irregular and rapid electrical activity in the atria, leading to an irregular ventricular response. Timely and accurate diagnosis of A-fib is crucial for appropriate management and treatment. One of the primary diagnostic tools used is the electrocardiogram (ECG), which captures the heart’s electrical activity. This section discusses the process of diagnosing A-fib using an ECG.
1. Recording the ECG:
To begin the diagnostic process, healthcare professionals attach electrodes to specific positions on the patient’s chest, limbs, and torso. These electrodes detect and record the electrical signals produced by the heart.
2. Assessing P Waves:
In a normal ECG, each heartbeat is preceded by a P wave, which represents atrial depolarization. However, in A-fib, the P waves are absent because the atria are fibrillating. Instead, irregular and rapid fibrillation waves, known as f waves, are observed on the ECG.
3. Identifying Irregular Rhythm:
A key characteristic of A-fib is an irregularly irregular rhythm. The distance between the f waves varies, resulting in an irregularly spaced ventricular response. This irregularity can be visually observed by analyzing the R-R intervals on the ECG.
4. Determining Ventricular Response Rate:
A-fib often leads to a rapid ventricular response due to the irregular conduction of atrial impulses to the ventricles. Healthcare professionals can calculate the ventricular response rate by measuring the distance between consecutive R waves (R-R intervals) and determining the heart rate in beats per minute (bpm).
5. Detecting Associated Abnormalities:
While diagnosing A-fib, healthcare professionals also check for other associated abnormalities that may affect the ventricular rate or indicate underlying heart conditions. These abnormalities may include atrioventricular blocks or bundle branch blocks, which can be identified by analyzing the ECG waveform.
6. Consulting a Healthcare Professional:
Interpreting an ECG and making a definitive diagnosis of A-fib should be done by a trained healthcare professional, such as a cardiologist or electrophysiologist. They consider the ECG findings in conjunction with the patient’s clinical history, symptoms, and other diagnostic tests to ensure an accurate diagnosis.
In conclusion, the ECG is a valuable tool in diagnosing A-fib. By analyzing the absence of P waves, identifying irregular rhythm, determining ventricular response rate, and detecting associated abnormalities, healthcare professionals can make an accurate diagnosis. It is crucial to recognize that the interpretation of an ECG and diagnosis of A-fib should be performed by qualified healthcare professionals to ensure optimal patient care and appropriate treatment planning.
Treatment Of A-fib
The treatment of atrial fibrillation (A-fib) aims to restore normal heart rhythm, prevent complications, and improve the patient’s quality of life. Various approaches can be employed based on the individual’s condition and preferences.
One common treatment option is electrical cardioversion, which involves delivering a controlled electric shock to the heart to restore normal rhythm. Another approach is catheter ablation, a procedure where a flexible, thin tube is inserted into the heart to eliminate abnormal electrical signals causing A-fib. Lifestyle modifications play a crucial role in managing A-fib and include maintaining a healthy weight, engaging in regular exercise, moderating alcohol and caffeine consumption, and managing stress levels. In certain instances, the utilization of blood-thinning medications may be imperative to prevent blood clots and minimize the risk of stroke.
Furthermore, individuals with A-fib may require treatment for underlying conditions like high blood pressure or thyroid disorders. The treatment approach is customized for each person, incorporating a combination of interventions to attain the optimal outcome. Regular monitoring and follow-up appointments with healthcare providers are essential to ensure treatment effectiveness and make any necessary adjustments.
By adopting a comprehensive approach to treatment, individuals with A-fib can effectively manage their condition and improve their overall well-being.
The Crucial Role That Early Diagnosis Plays In A-fib Treatment
Early diagnosis of atrial fibrillation (A-fib) is crucial to mitigate the associated risks and improve patient outcomes.
A-fib increases the risk of stroke and worsens heart failure, emphasizing the importance of timely detection and management. Early identification allows for the prescription of anticoagulants to prevent stroke and improves heart function through appropriate treatments. It also helps address symptoms like palpitations and fatigue, enhancing daily functioning. Additionally, early diagnosis helps prevent complications such as pulmonary embolism and peripheral arterial disease. Lifestyle modifications can further reduce risks, and early detection enables patient education on these changes.
ECG – the Gold Standard in A-fib diagnosis
A-fib can be episodic or asymptomatic, making early detection challenging. Wearable devices like smartwatches and fitness trackers equipped with photoplethysmography (PPG) sensors offer the potential for identifying paroxysmal or asymptomatic A-fib. These devices calculate irregular pulse rates from PPG data to infer A-fib diagnosis, emphasizing the importance of optimizing data algorithms to promote their widespread use. ECG remains the gold standard for diagnosing A-fib due to several reasons:
1. Direct measurement of electrical activity involves the use of an electrocardiogram (ECG), which records the heart’s electrical signals generated during each heartbeat. This provides a precise and detailed representation of the heart’s rhythm and can accurately detect irregularities associated with A-fib.
2. Well-established diagnostic tool: ECG is a widely used and accepted diagnostic tool for assessing cardiac conditions, including A-fib. It has been extensively studied and validated, making it a trusted method in clinical practice.
3. Higher sensitivity and specificity: Studies have demonstrated that ECG exhibits higher sensitivity and specificity in detecting A-fib in comparison to PPG. The electrical signals captured by ECG allow for more accurate identification of irregular heart rhythms characteristic of A-fib, reducing the risk of false positives or negatives.
4. Ability to capture complex waveforms: ECG records a range of waveforms, such as P-waves and QRS complexes, providing detailed information about the different phases of the cardiac cycle. This enables healthcare professionals to assess the severity and pattern of A-fib, which is essential for appropriate treatment planning.
5. Diagnostic criteria and guidelines: Diagnostic criteria and guidelines for A-fib are primarily based on ECG findings. These criteria have been developed over time through extensive research and clinical experience, further supporting the accuracy and practicality of ECG in diagnosing A-fib.
While PPG has its advantages, such as being non-invasive and easily accessible through wearable devices, it relies on measuring changes in blood volume using light sensors, which may be influenced by external factors and have limitations in accurately detecting irregular heart rhythms. Therefore, ECG remains the gold standard for diagnosing A-fib due to its direct measurement of cardiac electrical activity, established reliability, and higher accuracy in detecting this specific arrhythmia.
Wearable ECG Devices and the Diagnosis of A-fib
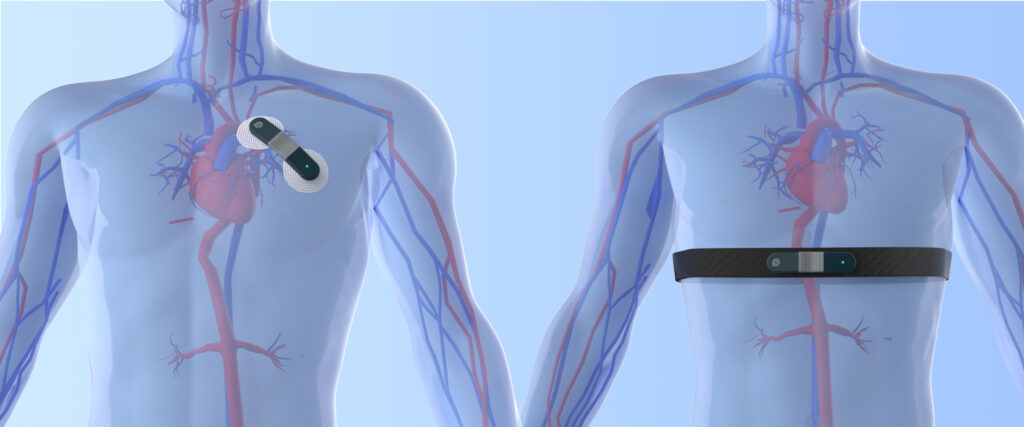
Wearable ECG devices for A-fib diagnosis are gaining popularity in the medical field. These devices combine ECG and wearable technology to provide convenient and continuous monitoring solutions.
The key advantage of wearable ECG devices is their portability and comfort. They are small, lightweight, and can be directly worn on the body, eliminating the need for uncomfortable electrodes. This allows patients to carry out their daily activities while being continuously monitored.
Wearable ECG devices offer the capability of continuous monitoring, unlike traditional ECGs that provide short-term monitoring. This continuous monitoring is particularly important for conditions like A-fib, which are intermittent and difficult to capture with traditional methods.
The market prospects for wearable ECG devices in A-fib diagnosis are significant. A-fib is a common cardiac arrhythmia, and with the aging population, its prevalence is increasing. Wearable devices provide opportunities for early diagnosis and treatment, reducing the risk of complications.
In conclusion, wearable ECG devices provide portability, comfort, and continuous monitoring, making them valuable for AF diagnosis. With the increasing prevalence of A-fib and the need for early detection, the market for these devices is expected to expand in the upcoming years.
Conclusion
Getting an early diagnosis for A-fib, as well as other cardiovascular conditions is essential. This helps to ensure you take action before serious complications develop. Having ECG monitors at home is definitely a good solution, as this allows you to easily detect problems with your heart rhythm and the cardiovascular system. Viatom offers a range of ECG devices that can aid in diagnosing A-fib while still at an early stage. Since 2013, Viatom has produced a number of healthcare devices that can be useful for detecting health-related problems at home and makes it easy to send reports to a healthcare provider.
For health monitors, look no further than Viatom.
References:
https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.120.31634
https://www.heartrhythmjournal.com/article/S1547-5271(20)30595-6/fulltext